Jacqui Rose, CEO of Pinnacle Revenue & Bryan Johnson, CEO of WeInfuse talk about Aduhelm Billing with support from Paige Bigley, Client Success, Product & Integrations at WeInfuse
Disclaimer: This blog article is merely a resource and shall not be considered professional Aduhelm billing advice. Use the advice outlined herein at your own risk.
Aduhelm Billing: The FDA has granted accelerated approval for ADUHELM for the treatment of Alzheimer’s disease, but now what? We know what disease the medication is used for, how it is administered, how often it is administered, but how do we create and bill the claim for Aduhelm? Many newly approved medications have challenges when it comes to billing them for the very first time. Aduhelm is already causing some confusion for many providers as it has multiple complexities that make it challenging to bill.
- Aduhelm has 2 NDC’s for two different strengths: 170mg and 300mg vials
- The dosage is weight-based (10mg/kg) and will fluctuate from patient to patient
- Most treatment will have some amount of wastage that needs to be billed
- There is no permanent HCPCS code at this time
The good news is Aduhelm is not the first newly approved drug to be released with these complexities. This article will attempt to guide billers through each of the steps needed to bill their first Aduhelm claim based on what we understand about the current medication and billing situation as of the time of this writing. In addition to reading this article closely and carefully, please also do your own research and make sure you have the most up-to-date information from the medication manufacturer (Biogen) and also the insurance company or Medicare/Medicaid you are sending the claim to.
Billing Miscellaneous HCPCS codes – J3490, J3590
As mentioned, Aduhelm is a newly FDA-approved medication; so, no permanent HCPCS code has been assigned. Therefore, billers must currently use a miscellaneous code, either J3490 or J3590, on Aduhelm claims. It is generally accepted by most commercial insurance companies and Medicare/Medicaid to use the J3590 code when billing biologic medications. In this article, we will stick with J3590, but billers should check with their insurance companies as updated policies are published in case they are expecting a J3490 code instead.
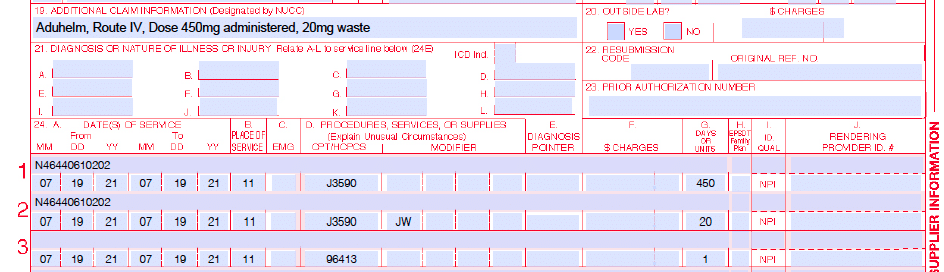
When billing any miscellaneous HCPCS code, Medicare and most commercial payers will want to see the “whole claim” information including the drug name, administered dose, wasted amount, as well as route of administration. It is a best practice to include this information in the Additional Claim Information area of the claim. Looking at a CMS-1500 form, this is box 19 as shown in our below example:
Standard HCPCS vs NDC Billing
Aduhelm is provided in 2 different vial sizes: strength of 170mg and 300mg. It will be very common for most patients to receive multiple vials and often a combination of the 2 different sized vials. In addition, it will be very common to have some amount of wastage with this treatment.
It is important to stop here before moving on and address the reality that there are 2 different billing methods to consider prior to putting charge lines on a claim. In Medical benefit billing, there are 2 ways to bill for medications.
- Standard HCPCS billing
- NDC Billing
I don’t really know if the first method is really called the “Standard” way, but it is the way billers have always billed for medications prior to NDC billing. The main differentiator between the two methods is that with the Standard method, there is only ever 1 charge line for a medication and 1 charge line for wastage (if applicable) regardless of the number of different vials used in the treatment.
With the NDC billing method, there is a different charge line for each specific medication vial used in the treatment. Each one of those vials with a unique NDC gets its very own line. There are also additional lines for any wastage if wastage is documented on the treatment. For a crash course on NDC Billing, check out this article: NDC Billing for Infusion and Injectable Medications
Some insurance companies, like UnitedHealthcare, have blanket requirements that all medications be billed using the NDC billing method. Other payers may or may not have these requirements and may or may not optionally accept NDC billing for claims. Medicare, for example, allows and encourages NDC billing but it is not required as of the date of this writing.
Both methods are outlined below. Please pay close attention to which method you will use when billing for Aduhelm because it will make a noticeable difference in how the final claim looks.
Aduhelm Billing Examples
I prefer real-world examples so let’s do some here. Our example patient has just completed a treatment where they received a 450mg dose of Aduhelm over 1 hour (60 minutes first-drip to last-drip). The patient weight was 100lbs or 45kg receiving a 10mg/kg dose. In order to utilize the different vial sizes most efficiently, the medication was prepared using:
- Qty: 1 of ADUHELM 170 MG/1.7 ML VIAL – NDC 64406010101
- Qty: 1 of ADUHELM 300 MG/3 ML VIAL – NDC 64406010202
This vial selection means a vial selection of 470mg’s total with 20mg’s of wastage. For Standard HCPCS billing, the charge lines would look like this below:
Standard HCPCS Billing
| Line | Code | Units | Modifier | Line Note |
| 1 | J3590 | 450 | 64406010202 | |
| 2 | J3590 | 20 | JW | 64406010202 |
| 3 | 96413 | 1 |
For J3490, J3590 – there is a bit of discussion and gray area going around about whether the Units should be the lowest unit (as shown above) or the unit should always = “1”. In the above example, I used 1 unit = 1 mg. Please check with your commercial insurance company, local Medicare MAC, or Medicaid agreements to find out what is expected in your specific situation.
For Standard HCPCS billing, you typically combine all the lines with the same HCPCS or CPT code and sum the units. Since there is only one line, you only have room for a single Line Note. In this case, I have added the NDC number as my Line Note. Even though we used 2 different NDC’s for this date of service/treatment, we only have room for 1 of them so we pick the largest vial size.
Looking at a paper claim on the CMS-1500 form, you should have something like this below for an example Date of Service of 7/19/2021:
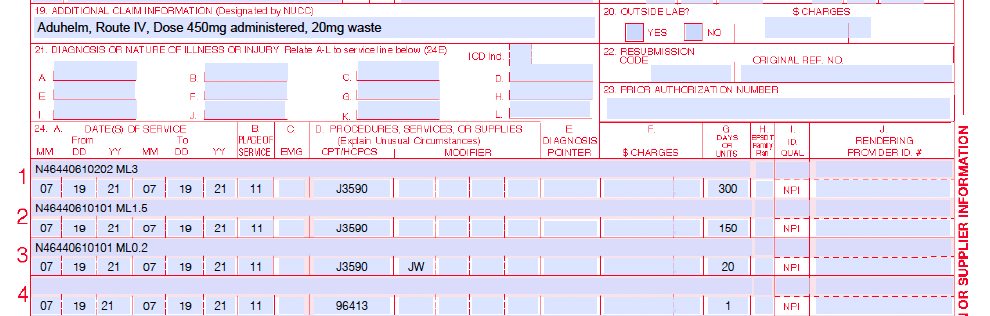
NDC Billing
For NDC Billing, the charge lines would look like this below:
| Line | Code | Units | Modifier | Line Note |
| 1 | J3590 | 300 | N464406010202 ML3 | |
| 2 | J3590 | 150 | N464406010101 ML1.5 | |
| 3 | J3590 | 20 | JW | N464406010101 ML0.2 |
| 4 | 96413 | 1 |
If you are already experienced with NDC Billing or you took the time to review our NDC Billing Blog, then this should look familiar to you. Note, that each different size vial with a different NDC is placed on its very own charge line and the wastage modifier (JW) is placed on the specific vial the waste came from.
Looking at a paper claim on the CMS-1500 form, you should have something like this below for an example Date of Service of 7/19/2021:
In both of these examples, I added a single CPT line of 96413 – Chemotherapy administration, intravenous infusion technique, up to one hour, single or initial substance
Many commercial payers will likely reimburse the 96413 for the infusion administration of Aduhelm as a biologic, but many may not so please check with your insurance company, local Medicare MAC, or Medicaid agreements to find out what is expected in your specific situation. If 96413 is not allowed, then you would use 96365 instead. For a breakdown of CPT billing, take a quick read here if you are not already familiar with the infusion billing hierarchy. The Confusion of Infusion Billing
Final Thoughts
As with any new specialty medication launch, information at the beginning is scarce and the situation is constantly changing. The key to success when billing these new medications is to stay in close contact with both government and private commercial payers and to keep yourself and your team as up-to-date as possible. Watch your first claims closely and follow up often to check on the status of these claims so you and your billing team can adjust your billing procedures accordingly.
With any luck, many of the payers will begin to finalize their payment policies for Aduhelm soon. Sometime in 2022, a permanent HCPCS code will hopefully be issued and this will reduce some of the complexity of billing these treatments.
Aduhelm is an exciting new medication bringing hope to many patients, families, and caregivers around the country. With some patience and attention to detail, your team can be a part of this treatment revolution and solution for these Alzheimer’s patients in your area.
Our Shameless Plug
If all of the above seems a bit daunting to you and you would rather not go through all of this for every new medication in the market, you could also just use WeInfuse. WeInfuse is an end-to-end workflow application designed for your provider-based infusion suite, stand-alone or pharmacy-based infusion center. WeInfuse automatically codes and calculates everything this article discusses so you and your team can focus on your patients.
If you are looking for a smart team to take care of all of this billing and complexity for you, then look no further than Pinnacle Revenue Management. The Pinnacle team is engaged daily with many, many infusion sites across the country and they have years of billing experience to bring to your business.
Disclaimer: This blog article is merely a resource and shall not be considered professional billing advice. Use the advice outlined herein at your own risk.
Guest Authors:
President and CEO at Pinnacle Revenue Management, Inc., Jacqui Rose has an extensive background in revenue management and software implementation. Prior to joining Pinnacle, Jacqui was a Reimbursement Manager for a home infusion reimbursement company.
Bryan Johnson, Co-Founder & CEO of WeInfuse, and CEO of RxToolKit, has dedicated his career to addressing and overcoming the challenges of the infusion delivery model. He is also a founding member of the National Infusion Center Association (NICA), and now serves as a Board Member.
Paige Bigley is the Director of Product & Integrations at WeInfuse. She has completed research over the Drug Supply Chain and Security Act, and has experience with vial scanning. As a former member of the Client Success and Integrations Team at WeInfuse, Paige is experienced in supporting clients using vial scanners for inventory check and inventory tracking within the treatment note.