Pre-Treatment
Workflow
WeInfuse can help your team organize and complete all required pre-treatment steps prior to every infusion appointment. Protect your patients and your bottom line, all while easing the burden on your office teams.

Pre-Treatment Features
Automated Electronic Insurance Eligibility and Benefits
WeInfuse has an automated electronic eligibility checking feature that allows you to quickly check eligibility for connected payers. Electronic eligibility checks determine whether coverage for a patient is active and returns pertinent benefit information for the patient’s current remaining co-pay, co-insurance, deductible, out-of-pocket, and effective term dates. This data is used in our Patient Responsibility Estimator and in other modules to ease the burden of checking this information manually with multiple insurances.


Insurance Verification Workflow
With WeInfuse, it’s easy to uncover and document pivotal patient details such as network status, coverage, authorization and referral requirements, and more. Our Verification tool simplifies the benefits investigation process by guiding users through questions to ask during a verification call, as well as providing a detailed view of order details, insurance, and benefits information.
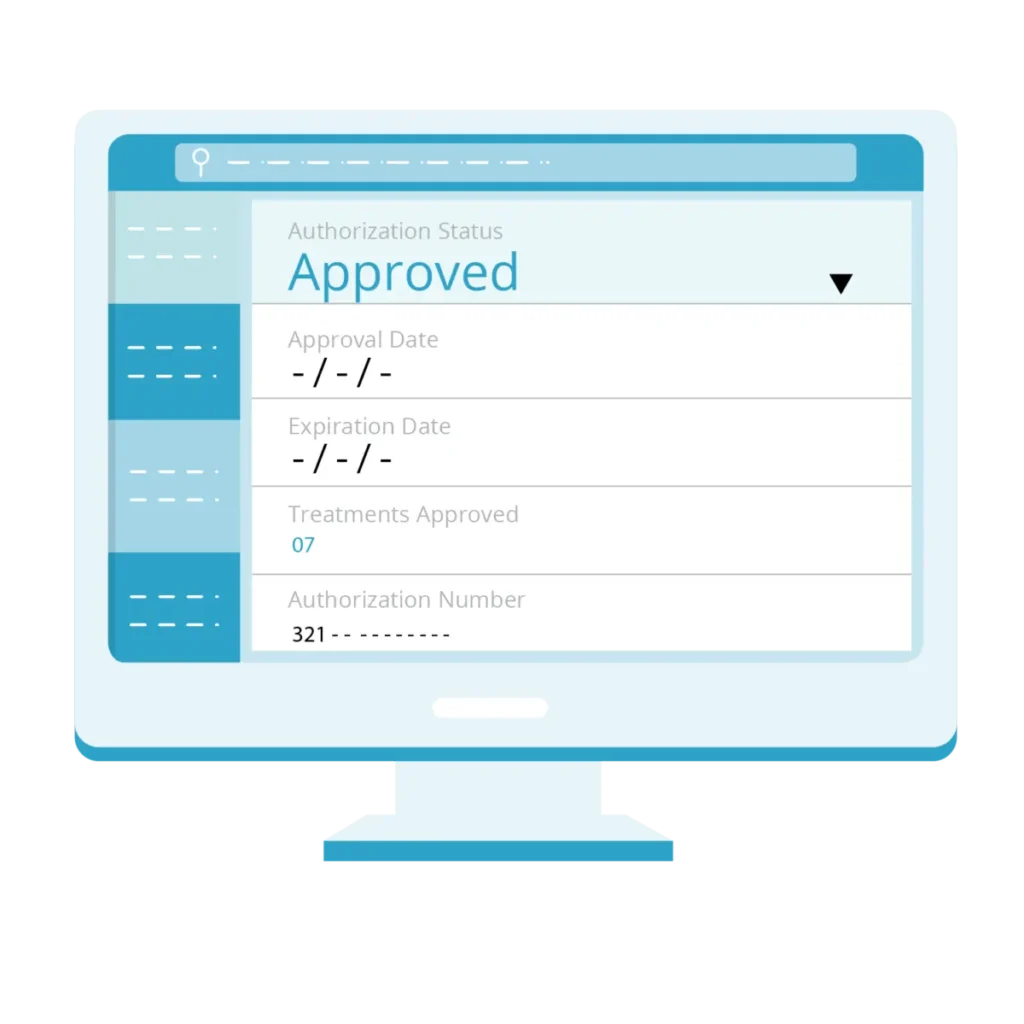
Authorizations, Referrals, Clinical and Financial Reviews
WeInfuse helps your intake team manage and prioritize intake tasks such as authorizations, referrals, clinical and financial reviews. Each of these tasks has their very own tracking and logging features to ensure that no patient is ever treated without a current authorization or active insurance. Our Scheduling and Treatment Note features also prevent your team from treating patients before intake tasks are effective and complete.

Patient Flow Task Management System
We know that managing a long list of pre-treatment and follow-up patient tasks is one of the most challenging aspects of operating an infusion center. Our Patient Flow tool simplifies and improves pre-treatment workflow by allowing your team to sort, filter, and prioritize verifications, authorizations, referrals, clinical and financial reviews, and scheduling tasks based on patients’ scheduled or target appointment date.
