What Infusion Providers should know about the Drug Supply Chain Security Act and Track and Trace
If you operate your own in-office infusion suite, or stand-alone infusion center, you already know that inventory management is a significant part of running a successful and profitable operation. Despite knowing this, at most infusion centers, medications are often inefficiently or ineffectively tracked. This makes it more difficult to determine which patient received a specific unit of medication on any historical treatment record. For those staying in the know, there are some evolving regulations and updates coming your way that should help everyone in the system better source, track, and manage their medication inventories.
For the last several years, the government and involved stakeholders have been working on new regulations to better label and track medications from the time of manufacture through the delivery of an individual medication to a patient.
This update is typically called “track and trace” and was established by the Drug Supply Chain Security Act or DSCSA. This blog post should help you get a solid overview of the DSCSA and prepare you and your team to both be compliant with and take advantage of these coming changes.
What is the Drug Supply Chain Security Act (DSCSA)?
In November of 2013 Congress passed the Drug Quality and Security Act (DQSA) to regulate and monitor drug manufacturing. Title II of the DQSA is the Drug Supply Chain Security Act, which outlines a plan to “build an electronic, interoperable system to identify and trace certain prescription drugs as they are distributed in the United States.”
The DSCSA outlines steps to achieve this electronic, interoperable system by November of 2023, with the goal that improved medication tracing and information exchange will allow individuals in all areas of the supply chain from manufacturers, to distributors, to dispensers, to more easily identify suspect products and facilitate recalls.
As part of the DSCSA, and beginning in 2017, manufacturers are now required to include an identifier on their drug packaging that is unique and traceable down to the unit level.
Which medications are labeled?
The DSCSA establishes that all “homogenous cases,” which are cases containing products with the same NDC and lot number, should have a product identifier. Additionally, all packages or the “smallest individual saleable unit of a product for distribution” and each “individual saleable unit” or the “smallest container of product … intended by the manufacturer or repackager for individual sale to a dispenser” should have their own product identifier.
What information do these identifiers include?
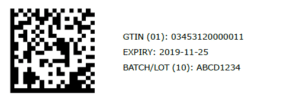
These product identifiers are a “standardized graphic that includes, in both human-readable form and on a machine readable data… the standardized numerical identifier, lot number, and expiration date of the product.”
Human Readable Labels
If you’ve looked at medication packaging recently, then you know that you can easily identify and interpret vial size, strength, lot number, and expiration date information from that packaging, the human readable product identifiers.
Machine Readable Labels
To simplify that term, the machine readable identifier on these medications, is their barcode.
You might have noticed that some medication packages have more than one barcode. The DSCSA calls for 2D Datamatrix codes on packages and either 2D Datamatrix codes or linear codes on homogenous cases. These linear codes that you’d find on a homogenous case of a medication are probably what you picture when you think of a barcode. They’re a stacked set of lines of varying thicknesses in a square or rectangular shape.
2D GS1 Datamatrix Codes
2D Datamatrix codes are a little different, and you might be unfamiliar with them unless you’ve been using WeInfuse’s vial scanning capabilities. 2D Datamatrix codes are squares or rectangles, composed of distinct shapes rather than entirely of lines. These 2D Datamatrix codes also contain more information than linear barcodes and house the following datapoints about the products they identify: GTIN (which contains the product’s NDC and other identifying information), Serial Number, Lot Number, and Expiration Date. These codes look like the image below.
To understand exactly how specific the information in a 2D Datamatrix code is, it’s helpful to reference GS1’s “Frequently Asked Questions (FAQs) by the Pharmaceutical Industry in Preparing for the U.S. DSCSA.” GS1 is the international, non-profit organization that maintains standards for 2D Datamatrix codes and their FAQ document outlines the differences between GTINs and NDCs, how serial numbers are generated, the basics of GS1 Datamatrix codes, and more.
For our purposes now, we’ll look at how these 2D Datamatrix codes function as unique product identifiers that enable manufacturers, distributors, and dispensers to track and trace medications. In terms of the information found in these codes, you’re probably familiar with identifying information like NDCs, lot numbers, and expiration dates, but you may not be familiar with GTIN’s and Serial numbers.
What is a GTIN?
Unlike an NDC, a GTIN is a global trade item number. According to GS1, “The GTIN is used for trade items around the world. The NDC is only used to identify drugs, and only drugs subject to U.S. FDA regulation.” So, the GTIN helps the NDC become something that is globally more useful and identifies other items besides just drugs. What’s important to know is that the product NDC is actually part of the GTIN and is included in every 2D GS1 Datamatrix barcode.
What are Serial Numbers?
The serial number on a 2D GS1 Datamatrix consists of a unique, alphanumeric set of up to 20 characters. Basically, a serial number is a unique identifier for that very specific box of medication that you have in your hand. The serial number allows a saleable unit of medication to be identified beyond just the NDC, Lot, and Expiration Date, and allows that medication vial, bag, or syringe to be tracked all the way back to where it was manufactured.
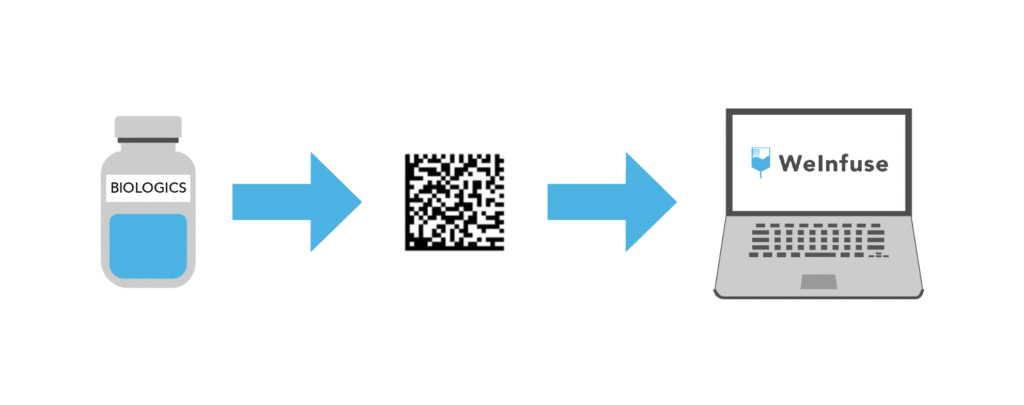
How does WeInfuse work with Inventory?
In WeInfuse, inventory is always tracked down to the NDC, lot number, and expiration date. In fact WeInfuse is one of, if not the only, last-mile system for inventory tracking, ensuring that in the case of a recall, you will be able to quickly and easily identify each patient who has been treated with inventory of a given lot number and expiration date. For clients using our vial scanning feature, inventory tracking is even more sophisticated and specific.
Vial scanning enables more than just time savings and inventory tracking at the lot number. Our planned updates for vial scanning will allow for inventory scanning directly into a patient’s treatment note. By allowing users to associate a specific vial or unit of inventory with a patient treatment, WeInfuse will be able to assign a specific medication, by serial number, to a patient’s treatment. Stay tuned for these new updates coming soon!
Future Outlook for Track and Trace and the DSCSA
While track and trace down to the patient administration level isn’t something that is currently written into the DSCSA, as the regulatory landscape evolves, we are certain that we will see reporting requirements for drug administration at the provider level. If and when such measures are established, WeInfuse vial scanning will easily and effectively enable this kind of drug administration tracking and reporting on a patient by patient basis.
If you want to learn more about the Drug Supply Chain Security Act, we believe the best resources are available through GS1. GS1 also offers provider-specific resources.
To learn more about how WeInfuse can help your teams create a fully tracked and patient reconciled inventory management system (track and trace), contact our team and we will be happy to help. Click here to request a demo.